The U.S. beats out other countries in many categories—and, increasingly, obesity is one of them.
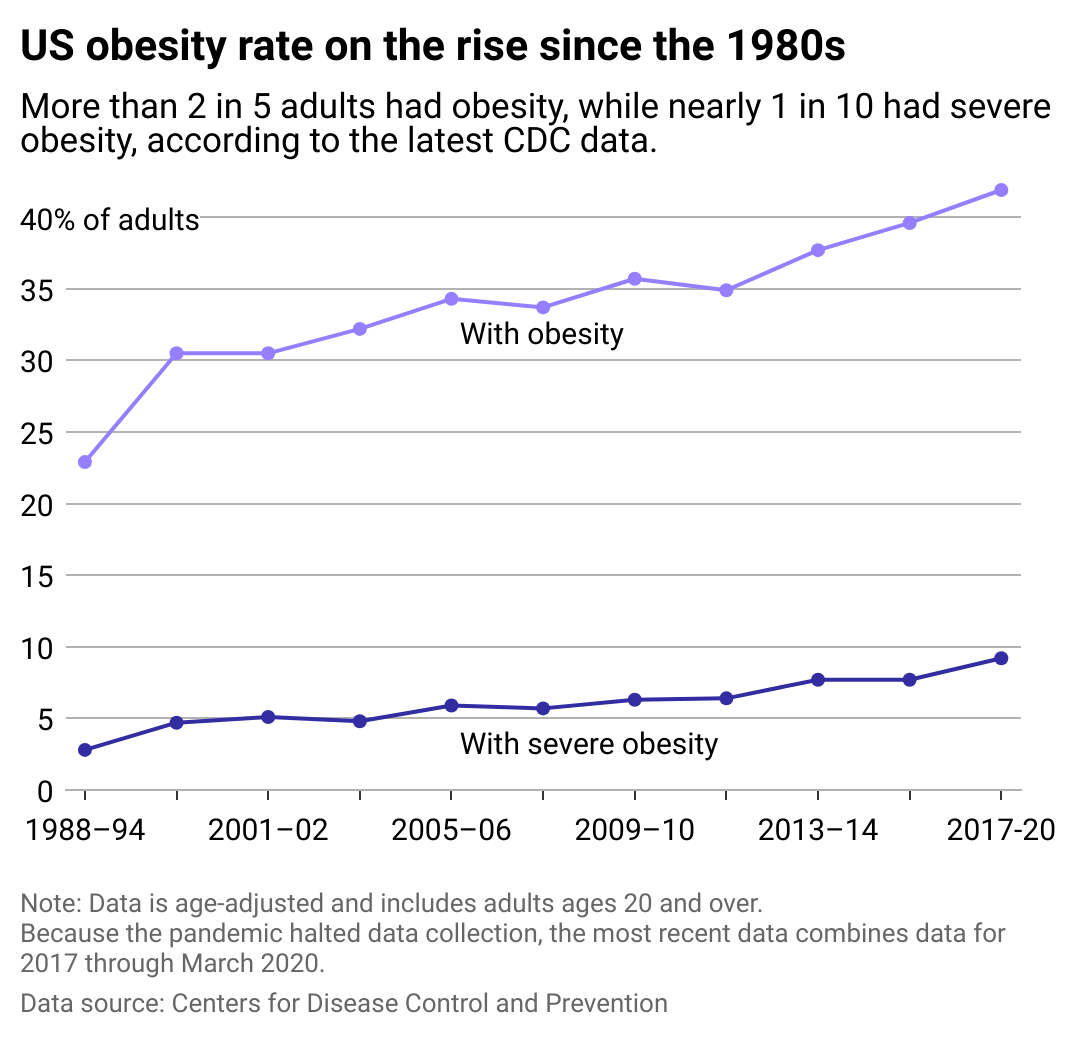
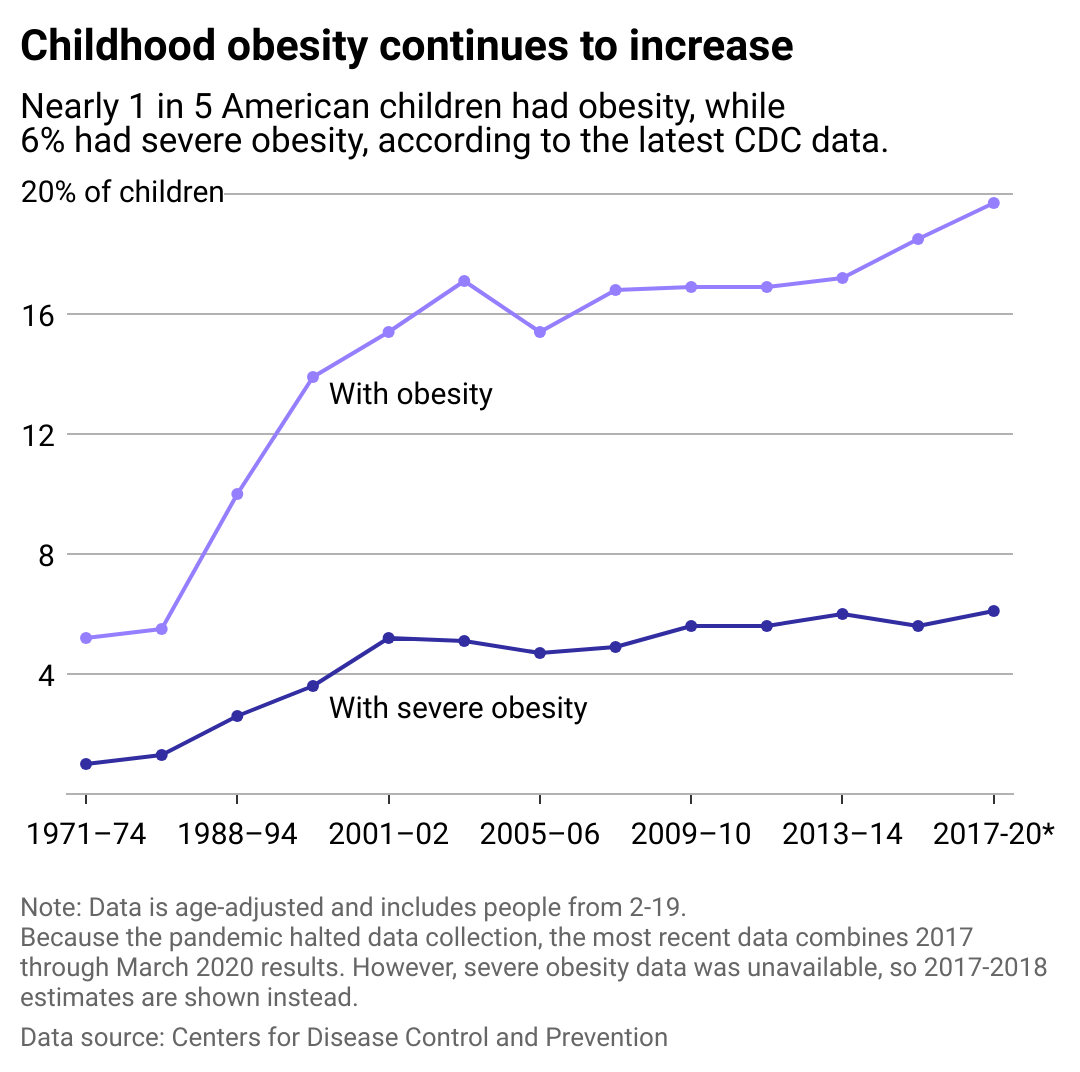
Live It Up used data from the Centers for Disease Control and Prevention to explore this public health problem and better understand long-term obesity trends in American children and adults. Rates were determined using the National Health and Nutrition Examination Survey, last released in 2021.
Recommended Videos
The World Health Organization defines obesity as “abnormal or excessive fat accumulation that presents a risk to health.” As of 2016, the United States ranks 16th globally for obesity rates, behind smaller countries in the South Pacific and Middle East, according to Our World in Data. A 2023 article in the journal Obesity Science Practice found that obesity rates in the U.S. have increased over 300% since the 1960s.
Obesity also increases the risk of comorbidities, including heart disease, diabetes, sleep apnea, and some types of cancer. Health issues can emerge when a person is slightly overweight and become more severe as their weight increases. Obesity also has links to premature death.
There are social dimensions of the condition, too. People with obesity face stigma from their peers, coworkers, and even their health care providers. Many people with obesity find that their health concerns are dismissed by professionals, who instead focus on their weight as the central reason for their ailments and on weight loss as the solution.
These factors are partly due to how obesity is calculated based on body mass index. WHO considers an individual with a BMI of 30 or over obese. While the BMI scale has been found helpful in describing population trends, it has received criticism for being inaccurate in telling the whole story about a person’s health. For instance, BMI does not distinguish between fat, bone, and muscle. The American Medical Association now recommends that providers de-emphasize the importance of BMI in assessing a patient’s health.
Obesity is complex—there’s more to it than a number on the scale.

KK Stock // Shutterstock
How health care policies work to fight obesity
The U.S. continues to try to curb this public health issue with legislation, health care policies, and a culture shift. On a federal level, the Treat and Reduce Obesity Act introduced in 2021 aims to expand Medicare access to obesity-specialized drugs and health care providers. State policies have included public messaging, physical activity programs in schools, and incentives for manufacturers to decrease sugar content in their products.
Similarly, in 2018, England introduced a public health initiative challenging the food manufacturing industry to reduce the calorie content of high-sugar and high-fat products by 20% by the end of 2024. The Organization for Economic Cooperation and Development—which includes 38 member countries—proposed promoting this project on a global scale. Unfortunately, according to research published by the Office for Health Improvement and Disparities in February 2024, little progress has been made in England's calorie reduction program, the timeframe for which has been extended to 2025 due to the COVID-19 pandemic.
Many of these strategies are not new, but the advent of drugs like Wegovy and Ozempic may transform the way we treat obesity. These drugs contain semaglutide, which reduces blood glucose and reduces appetite. Despite dramatic results, they are far from miracle cures.
Besides being prohibitively expensive and in short supply, the long-term sustainability of these treatments is unknown. A study published in a 2022 issue of the journal Diabetes, Obesity and Metabolism found that patients who stop using these drugs tend to regain about two-thirds of the weight lost within the next year.
These treatments are not just for adults. Since Wegovy approved use for adolescents in 2022, an increasing number of children have been prescribed the medication despite many unknowns about its long-term effects.
Live it Up
Adult obesity and changing habits in America
Numerous factors contribute to the startling obesity numbers. A soaring rise in the consumption of unhealthy foods and an increasingly sedentary lifestyle are two of the main culprits. One of the root causes is changes to the American diet in the late 1970s, with the introduction of ultra-processed foods containing more fat, sugar, and salt, sugar-sweetened beverages, and fewer whole foods.
For adults, it can be hard to stay active: In 2022, the World Health Organization reported that about 1 in 4 people globally do not get the amount of physical activity recommended by health agencies. The Department of Health and Human Services says adults should get at least 2.5 hours of "moderate-to-vigorous" activity weekly. And physical activity doesn't have to mean exercise—it can be anything that gets your body moving, even if it just means doing chores around the house.
According to 2021 research published by the International Journal of Environmental Research and Public Health, the COVID-19 pandemic, which caused many adults to start working from home, decreased overall physical activity. After surveying more than 13,500 people in 14 countries, researchers found a 41% reduction in moderate-to-vigorous physical activity and a 42% decrease in vigorous physical activity compared to pre-restriction numbers.
It turns out that daily commutes and just getting up to walk around the office play a bigger role in increasing our daily activity and weight overall than we might think.
Live it Up
How public policy affects childhood obesity and dietary trends
Childhood obesity can have a long-term impact on an individual's health and overall well-being. It can lead to lowered performance in school and increased bullying.
There's a reason childhood obesity spiked in the 1980s, according to Dr. Norman J. Temple, professor of nutrition at Athabasca University. Ultra-processed and high-sugar foods and fast food boomed in popularity around 1976. A series of Nixon-era farm bills made these options much cheaper, possibly contributing to their rise.
Since the school day and extracurricular activities offer ample opportunities for physical activity, children tend to have lower rates of obesity than adults. However, despite recommendations that youth engage in 60 minutes of physical activity daily, only two states—the District of Columbia and Oregon—currently meet these recommendations with their physical education programs, according to the American Public Health Association.
Schools also have an opportunity to decrease childhood obesity rates via nutrition. Increasing the amount of whole-nutrient foods in school lunches overall can benefit all demographics. A 2023 Trust for America's Health report states that focusing on programs like the National School Lunch Program and Supplemental Nutrition Assistance Program can help youth from lower-income households, who statistically have less access to affordable, healthy options.
A 2017 Harvard T.H. Chan School of Public Health study found that over 57% of children at that point would experience obesity at age 35. Researchers also found that higher weight in childhood can indicate a higher risk of obesity later in life.
Addressing childhood obesity early on is crucial for curbing cascading effects on the future population. Educating and developing healthy habits in youth can result in a lower adult obesity rate in the years to come.
Story editing by Shannon Luders-Manuel. Additional editing by Kelly Glass and Alizah Salario. Copy editing by Kristen Wegrzyn.
This story originally appeared on Live It Up and was produced and distributed in partnership with Stacker Studio.